Navigating the complex world of health insurance is a challenge for both patients and healthcare providers. In Ohio and Illinois—two states with diverse populations and healthcare networks—the challenges of insurance billing are amplified by state-specific Medicaid systems, varying payer requirements, and rapidly evolving federal regulations. For providers, ensuring that claims are submitted accurately, reimbursements are timely, and denials are minimized requires not just medical knowledge but also billing expertise.
1. Introduction
The healthcare revenue cycle begins long before a patient sets foot in a clinic—it starts with verifying insurance and ends with collecting payments. In between lies a maze of documentation, coding, compliance, and communication. For providers in Ohio and Illinois, managing this revenue cycle requires precise coordination between front-office staff, billing teams, and insurance companies.
Healthcare billing services have evolved from simple claim filing to comprehensive revenue cycle management systems that address insurance eligibility, credentialing, claim tracking, denial management, and patient billing. In states with different Medicaid structures and commercial payer landscapes, customized solutions are essential.
2. Overview of Health Insurance in Ohio and Illinois
Both Ohio and Illinois operate under the guidelines of the Affordable Care Act, but each state has taken unique paths with Medicaid expansion and managed care.
Ohio:
Expanded Medicaid in 2014.
Overseen by the Ohio Department of Medicaid (ODM).
3+ Managed Care Organizations (MCOs) such as Buckeye Health Plan, Molina, and CareSource.
Significant rural populations rely on Medicaid and telehealth.
Illinois:
Also expanded Medicaid under the ACA.
Administered by the Illinois Department of Healthcare and Family Services (HFS).
Operates under the HealthChoice Illinois managed care program.
Urban providers in Chicago often face higher claim volumes and complex payer mixes.
The presence of multiple commercial payers, Medicare Advantage plans, and Medicaid MCOs creates a multi-layered insurance ecosystem where billing precision is non-negotiable.
3. Common Insurance Billing Challenges
Providers in both states frequently experience insurance-related billing challenges, many of which stem from a lack of process alignment or knowledge of payer rules.
3.1. Inaccurate Eligibility Checks
If a patient’s insurance is not correctly verified before service, the claim may be denied.
3.2. Incomplete Documentation
Missing clinical notes, incorrect CPT/ICD-10 codes, or lack of prior authorizations often lead to payment delays.
3.3. Coordination of Benefits (COB) Confusion
Patients with multiple insurances can trigger claim denials due to incorrect primary/secondary payer information.
3.4. Changing Payer Requirements
Medicaid MCOs and commercial insurers often update billing rules, which providers must track proactively.
3.5. Denials and Appeals
Claim denials, particularly for non-covered services or improper documentation, can drag down cash flow unless appealed quickly and correctly.
4. The Role of Medical Billing Services
Medical billing companies act as a bridge between healthcare providers and insurance companies. Their role is essential in ensuring that services rendered are properly coded, claims are submitted correctly, and payments are collected efficiently.
Key Services Include:
Insurance eligibility verification
Claim submission and tracking
Coding audits and corrections
Denial management and appeals
Patient billing and collections
Compliance reporting
Providers in Ohio and Illinois increasingly rely on these services to offload administrative burdens and focus on patient care.
5. Medicaid and Managed Care Plans in Both States
Ohio’s Medicaid Structure:
The transition to Next Generation Managed Care emphasizes more personalized and coordinated care.
Providers must enroll and credential with ODM and the chosen MCOs.
Each MCO has its own billing rules, formats, and portals (e.g., Buckeye uses Availity).
Illinois’ Medicaid Structure:
Operates through Healthcare billing services in Ohio , with plans like Blue Cross Community Health, Meridian, and CountyCare.
Claims often require attachments or encounter data submission.
Providers must carefully monitor authorization policies, especially for behavioral health and long-term care.
Navigating these systems requires in-depth knowledge of specific Medicaid requirements. Billing services help reduce errors and track changing payer policies.
6. Insurance Credentialing and Payer Enrollment
Credentialing is the first step in being reimbursed by insurers. Without proper credentialing, claims will be denied regardless of coding accuracy.
Common Tasks:
Completing CAQH applications
Enrolling with Medicare and Medicaid
Managing re-credentialing timelines
Verifying participation in MCO networks
In Illinois, for example, providers must undergo IMPACT enrollment for Medicaid, while in Ohio, Medicaid enrollment is handled through the OH|ID system. These processes are time-consuming but critical.
Credentialing specialists within billing companies ensure that providers are properly linked to each payer system before claims are sent.
7. Preventing Claim Denials: Best Practices
Denials can drastically delay revenue cycles. Healthcare billing services implement denial-prevention strategies tailored to each payer’s preferences.
7.1. Accurate Patient Data Collection
From the first appointment call, verify:
Insurance ID numbers
Policy status
Referrals or authorizations
7.2. Real-Time Eligibility Checks
Use clearinghouse tools to confirm active coverage and deductibles.
7.3. Clean Claim Submission
Apply correct CPT/HCPCS and ICD-10 codes, modifiers, and units. Ensure NPI and taxonomy codes match.
7.4. Proactive Denial Tracking
Log denial reasons, analyze patterns, and appeal within payer-specific timeframes.
7.5. Staff Education
Keep front-desk and coding staff updated with payer newsletters and billing webinars.
8. Compliance and Legal Considerations
Billing practices must align with federal and state laws. Ohio and Illinois both have stringent requirements around Medicaid fraud, HIPAA, and billing transparency.
Key Regulations:
HIPAA: Protects patient data during billing processes.
False Claims Act: Penalizes fraudulent claims, intentional or not.
State-Specific Rules: Both states perform regular audits. Errors can result in recoupments and penalties.
Billing companies help mitigate compliance risks by:
Maintaining audit-ready documentation
Using encrypted billing platforms
Performing internal compliance audits
9. Patient Communication and Financial Transparency
With rising deductibles and copays, patients are bearing more of the healthcare cost burden. Clear communication and billing transparency improve collections and satisfaction.
Billing Services Can Help:
Provide cost estimates before service
Offer digital bills and payment options
Manage payment plans and reminders
Handle patient inquiries professionally
In areas like Columbus and Chicago, where diverse populations speak different languages, multilingual billing support is increasingly valuable.
10. Technology’s Role in Insurance Navigation
Modern medical billing services for mental healthcare Illinois leverage advanced technology to streamline every aspect of the insurance process.
Key Tools Include:
Practice Management Systems (PMS): Automate scheduling, billing, and reporting.
Clearinghouses: Interface with multiple payers for electronic claims and remittance.
AI-Powered Coding Assistants: Suggest accurate CPT and ICD-10 codes based on documentation.
Analytics Dashboards: Monitor claim status, denial rates, and financial KPIs.
Providers in Ohio and Illinois benefit greatly from centralized, cloud-based platforms that integrate billing, credentialing, and insurance workflows.
11. Case Studies from Ohio and Illinois
Case 1: Pediatric Practice – Cincinnati, Ohio
Challenge: Frequent claim denials due to improper coding.
Solution: Partnered with a billing service with pediatrics expertise.
Result: Denial rate reduced by 40% in 3 months; cash flow improved significantly.
Case 2: Behavioral Health Center – Peoria, Illinois
Challenge: Struggled with Medicaid MCO credentialing and delayed payments.
Solution: Outsourced to a billing firm experienced in HealthChoice Illinois.
Result: Successfully credentialed with all major MCOs; revenue grew by 22%.
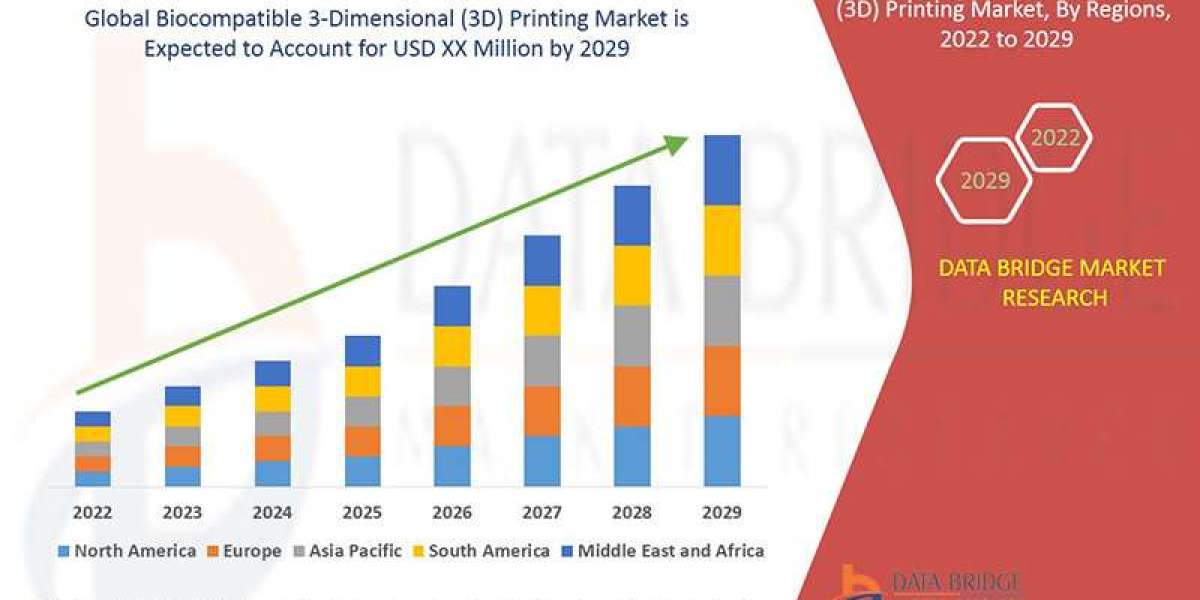
12. Future Outlook of Insurance Billing in Healthcare
The insurance billing landscape will continue to evolve in the coming years.
Predicted Trends:
More Value-Based Contracts: Billing services will need to report on quality metrics, not just fee-for-service.
Real-Time Claims Processing: Instant payer responses will reduce wait times for adjudication.
Automated Appeals Management: AI will handle denial reprocessing at scale.
Patient-Friendly Billing Models: Simpler invoices, upfront cost estimators, and mobile payment tools will be the norm.
In Ohio and Illinois, where patient populations and payer structures are dynamic, staying ahead of these trends is key to long-term practice success.
13. Conclusion
Navigating insurance in today’s healthcare climate is a full-time job—especially in states like Ohio and Illinois with layered payer systems, diverse patient populations, and unique Medicaid structures. Healthcare billing services have become essential partners in helping providers overcome these challenges.
By streamlining processes such as eligibility verification, claim submission, credentialing, and patient billing, medical billing professionals ensure practices get paid correctly and on time. Most importantly, they allow healthcare providers to focus on what truly matters—delivering exceptional care to their communities.
Whether you're an independent physician in Dayton or a specialty clinic in Springfield, partnering with expert billing professionals can transform your insurance challenges into opportunities for financial stability and growth.